The next group of disorders we
will look at are those that are associated with pustules. In the mnemonic it is simply
"II". "I" standing
for infective, either viral, bacterial or fungal, and occasionally rickettsial
or I standing for inflammatory, and with inflammatory it is usually either
drugs or psoriasis. There are other rarer inflammatory / immunological causes of pustules and we will deal with these a little bit later
in this presentation.
When one sees pustules histologically though, you are going to see them at different levels in the skin, in different conditions. Pustules basically represent a neutrophilic (rarely eosinophilic) collection and they may be subcorneal, they may be intraepidermal, they may be dermal, but most pustules in fact are going to be in the epidermis or subcorneal area. You can get pustules that are made up of eosinophils rather than neutrophils and there is a group of disorders that are associated with these eosinophilic pustules.
The quintessential viral pustular disorder is herpes simplex and it usually gives rise to a pattern of intraepidermal vesicles. There is necrosis of the keratinocytes because of the cytopathic effects of the virus with balloon degeneration of the keratinocytes. The other thing that you may notice histologically is acantholysis or separation of the cells. This again is due to the viral damage, but the important thing is to look for this balloon degeneration of the keratinocytes. This is the reason the intraepidermal lesions form in the first place. There is swelling of the cell and rupture. Sometimes herpes virus can be seen along the sides of hair follicles as well but again the same balloon degeneration will be seen. Often you can get some multi-nuclear giant cells and variation in the shape of the nucleus of degenerate cells because of oedema. Herpes zoster and Varicella virus give exactly the same histological features as the herpes simplex virus.
View this virtual slide of Herpes Simplex
The other viruses that can occasionally give a pustular eruption are Orf and Milker's nodules. They give almost a pseudo blister, although there can be small pustules on the surface, but histologically what you see depends on the stage of evolution of the lesion. These lesions usually evolve over a six to eight week period. They are due to a paravaccinia poxvirus that is picked up from young sheep or goats, generally when they are being fed. Histologically you will see again vaccuolation in the epidermis, but what you will see this time are pink inclusion bodies. Often there is full thickness necrosis of the epidermis and it is this that gives the impression of a blister. There is also quite marked vascular dilatation under these lesions, often with extravasated red blood cells as well and this is what gives the bright red colour to these lesions. There is often lymphocytic and neutrophilic infiltrate as well and it is the neutrophils that can play a part in pustule formation. A characteristic feature you should look for though is the dermal papillary oedema and this adds to the illusion that a blister is being formed here. Exactly the same pathology occurs with Milker's nodules.
View this Virtual Slide of Orf
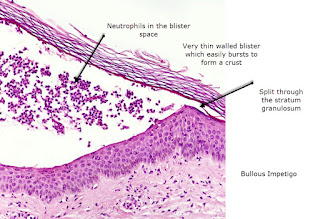
Pustules can also be a feature of bacterial infections particularly those associated with follicles, which is usually a staph folliculitis and those associated with staph impetigo, but often in these circumstances it is not so much pustules as oozing which is seen and crust formation. The histopathology in impetigo is accumulation of neutrophils in the subcorneal space and this is why the surface of these blisters or pustules is quite fragile. There is not really a thick covering of epidermis and so they tend to burst and form crusts very quickly. You should be able to see Gram positive cocci here and there will be an inflammatory infiltrate in the papillary dermis. If the staphylococcus is a toxin producing staph then you may get some acantholysis in the subcorneal space.
View this Virtual Slide of Impetigo
When one sees pustules histologically though, you are going to see them at different levels in the skin, in different conditions. Pustules basically represent a neutrophilic (rarely eosinophilic) collection and they may be subcorneal, they may be intraepidermal, they may be dermal, but most pustules in fact are going to be in the epidermis or subcorneal area. You can get pustules that are made up of eosinophils rather than neutrophils and there is a group of disorders that are associated with these eosinophilic pustules.
The quintessential viral pustular disorder is herpes simplex and it usually gives rise to a pattern of intraepidermal vesicles. There is necrosis of the keratinocytes because of the cytopathic effects of the virus with balloon degeneration of the keratinocytes. The other thing that you may notice histologically is acantholysis or separation of the cells. This again is due to the viral damage, but the important thing is to look for this balloon degeneration of the keratinocytes. This is the reason the intraepidermal lesions form in the first place. There is swelling of the cell and rupture. Sometimes herpes virus can be seen along the sides of hair follicles as well but again the same balloon degeneration will be seen. Often you can get some multi-nuclear giant cells and variation in the shape of the nucleus of degenerate cells because of oedema. Herpes zoster and Varicella virus give exactly the same histological features as the herpes simplex virus.
View this virtual slide of Herpes Simplex
The other viruses that can occasionally give a pustular eruption are Orf and Milker's nodules. They give almost a pseudo blister, although there can be small pustules on the surface, but histologically what you see depends on the stage of evolution of the lesion. These lesions usually evolve over a six to eight week period. They are due to a paravaccinia poxvirus that is picked up from young sheep or goats, generally when they are being fed. Histologically you will see again vaccuolation in the epidermis, but what you will see this time are pink inclusion bodies. Often there is full thickness necrosis of the epidermis and it is this that gives the impression of a blister. There is also quite marked vascular dilatation under these lesions, often with extravasated red blood cells as well and this is what gives the bright red colour to these lesions. There is often lymphocytic and neutrophilic infiltrate as well and it is the neutrophils that can play a part in pustule formation. A characteristic feature you should look for though is the dermal papillary oedema and this adds to the illusion that a blister is being formed here. Exactly the same pathology occurs with Milker's nodules.
View this Virtual Slide of Orf
Pustules can also be a feature of bacterial infections particularly those associated with follicles, which is usually a staph folliculitis and those associated with staph impetigo, but often in these circumstances it is not so much pustules as oozing which is seen and crust formation. The histopathology in impetigo is accumulation of neutrophils in the subcorneal space and this is why the surface of these blisters or pustules is quite fragile. There is not really a thick covering of epidermis and so they tend to burst and form crusts very quickly. You should be able to see Gram positive cocci here and there will be an inflammatory infiltrate in the papillary dermis. If the staphylococcus is a toxin producing staph then you may get some acantholysis in the subcorneal space.
View this Virtual Slide of Impetigo
Pustules due to fungi are usually
seen when steroids have been applied to the lesion and the steroids are then
withdrawn. An immune reaction occurs,
often giving rise to pustules in the advancing edge of the red scaly rash. They
also can be seen when an animal fungus is the dermatophyte responsible for
infections and there is a marked immune reaction to this. This is particularly common in the scalp or
beard areas where it is known as a kerion.
The histopathology with a kerion is marked perifollicular neutrophils,
so it is a form of perifollicular infection that can be difficult to
distinguish between a severe staph infection and the inflammation you get to
an animal fungus. Often the degree of
destruction and the degree of inflammation reduces the number of hyphae and spores
that one may see in this condition.
View this Virtual Slide of Bullous dermatophytosis
Pustules centred around hair follicles on the lower legs can be what is known as Majocchi's granuloma and the histopathology here is of perifollicular and dermal granulomas. If there is enough inflammation though some pustules can form on the surface but the histopathology is of an infection deep down in the dermis following a hair follicle down deep with rupture of the hair follicle due to the fungal infection and granuloma formation.
View this Virtual Slide of Majocchi's Granuloma
Candidiasis is often a secondary infection seen in flexural disorders such as psoriasis and intertrigo and some satellite lesions are seen in the surrounding skin. These pustules are made up of neutrophils in the stratum corneum or in a subcorneal distribution, but you should be able to see pseudohyphae budding yeasts in the stratum corneum as well indicating the yeast basis or the fungal basis for this infection, but again the inflammation is centred high either in or just under the stratum corneum itself. In the rare variant chronic mucocutaneous candidiasis, where there is an immune deficiency causing failure to mount an immune reaction to candida, then the histology is similar to superficial candidiasis but there is more epidermal acanthosis and spores and hyphae were easily found. Occasionally deep fungi will rupture onto the surface of the skin in an extravasation phenomenon and give rise to perilesional pustules, but the histopathology here will show the dermal granulomas and dermal abscesses associated with this type of condition and special stains may pick up the relevant fungus as in sporotrichosis and in chromoblastomycosis.
View this Virtual Slide of Candidiasis
View this Virtual Slide of Bullous dermatophytosis
Pustules centred around hair follicles on the lower legs can be what is known as Majocchi's granuloma and the histopathology here is of perifollicular and dermal granulomas. If there is enough inflammation though some pustules can form on the surface but the histopathology is of an infection deep down in the dermis following a hair follicle down deep with rupture of the hair follicle due to the fungal infection and granuloma formation.
View this Virtual Slide of Majocchi's Granuloma
Candidiasis is often a secondary infection seen in flexural disorders such as psoriasis and intertrigo and some satellite lesions are seen in the surrounding skin. These pustules are made up of neutrophils in the stratum corneum or in a subcorneal distribution, but you should be able to see pseudohyphae budding yeasts in the stratum corneum as well indicating the yeast basis or the fungal basis for this infection, but again the inflammation is centred high either in or just under the stratum corneum itself. In the rare variant chronic mucocutaneous candidiasis, where there is an immune deficiency causing failure to mount an immune reaction to candida, then the histology is similar to superficial candidiasis but there is more epidermal acanthosis and spores and hyphae were easily found. Occasionally deep fungi will rupture onto the surface of the skin in an extravasation phenomenon and give rise to perilesional pustules, but the histopathology here will show the dermal granulomas and dermal abscesses associated with this type of condition and special stains may pick up the relevant fungus as in sporotrichosis and in chromoblastomycosis.
View this Virtual Slide of Candidiasis
"I" also stands for
inflammatory and inflammatory pustules can be due to drugs or to pustular
psoriasis. Pustules at the edge of an
advancing area coming out from flexures or the groin can also be a feature of
necrolytic migratory erythema and of Sneddon Wilkinson Syndrome and pustules
can also be seen around the oral and peri-anal red scaly lesions of
acrodermatitis enteropathica. In subcorneal
pustular dermatosis you have, as the name suggests, a pustule in the subcorneal
area and it is made up of neutrophils but it is often described as sitting on
the epidermis. There is no depression
into the epidermis and it is quite a characteristic picture. Subcorneal pustular dermatosis is also known
as Sneddon Wilkinson Disease and it is like an IgA pemphigus but with negative
DIF typically involving intertriginous areas on the trunk but sparing the
face. It is usually associated with an
IgA gammopathy.
View this Virtual Slide of Sub corneal Pustular Dermatosis
View this Virtual Slide of Sub corneal Pustular Dermatosis
Pustular psoriasis is
characterised by intraepidermal pustules, rather than subcorneal
pustules. There are usually a lot of
neutrophils to be seen as an inflammatory infiltrate in the papillary dermis,
but they go into the epidermis as well.
Subcorneal pustules can form and they are overlayed with a thin roof of
stratum corneum. There are usually no
eosinophils in pustular psoriasis. Again
there may be some degree of psoriasiform acanthosis and hyperplasia of the
epidermis. It depends on the
circumstances in which this condition occurs.
View this Virtual Slide of Pustular Psoriasis
In palmar plantar pustulosis, the localised pustular psoriasis of the palms and soles, there is usually a very thick stratum corneum overlying the pustule. These pustules are often quite stable and gradually resolve and form a brown crust. This crust is a parakeratotic scale crust that subsequently falls off.
The other clinical variants of pustular psoriasis are the generalised Von Zumbush variant with acute systemic symptoms including fever and explosive onset.
Impetigo herpetiformis, is a pustular variant of psoriasis occurring in pregnancy.
Acropustulosis or acrodermatitis of Hallopeau, which is seen on the tips of the fingers and around the nails often causing quite marked dystrophy of the nails. Reiters syndrome can also give rise to very similar histopathology to localised pustular psoriasis of the palms and soles with psoriasiform epidermal hyperplasia and a thick overlying stratum corneum layer. The two can be histologically indistinguishable from localised pustular psoriasis. The glucagonoma syndrome gives rise to necrolytic migratory erythema and again this looks somewhat like Sneddon Wilkinson Syndrome with a spreading lesion coming out of the flexures with pustules at the edge, but the pustules are really quite fragile. This is due a glucagon secreting tumour of the pancreas. The rash is typically seen in the perineum, buttocks and groin. You get a psoriasiform hyperplasia but a classic feature is pallor of the cells of the upper epidermis and this same picture is also seen in acrodermatitis enteropathica and they may have common neutritional deficiency based etiologies. There is usually parakeratosis overlying this pallor and sometimes some subcorneal splits. If neutrophils invade the subcorneal splits it gives rise to the pustules at the advancing edge of these lesions.
View this Virtual Slide of Necrolytic Migratory Erythema
View this Virtual Slide of Pustular Psoriasis
In palmar plantar pustulosis, the localised pustular psoriasis of the palms and soles, there is usually a very thick stratum corneum overlying the pustule. These pustules are often quite stable and gradually resolve and form a brown crust. This crust is a parakeratotic scale crust that subsequently falls off.
The other clinical variants of pustular psoriasis are the generalised Von Zumbush variant with acute systemic symptoms including fever and explosive onset.
Impetigo herpetiformis, is a pustular variant of psoriasis occurring in pregnancy.
Acropustulosis or acrodermatitis of Hallopeau, which is seen on the tips of the fingers and around the nails often causing quite marked dystrophy of the nails. Reiters syndrome can also give rise to very similar histopathology to localised pustular psoriasis of the palms and soles with psoriasiform epidermal hyperplasia and a thick overlying stratum corneum layer. The two can be histologically indistinguishable from localised pustular psoriasis. The glucagonoma syndrome gives rise to necrolytic migratory erythema and again this looks somewhat like Sneddon Wilkinson Syndrome with a spreading lesion coming out of the flexures with pustules at the edge, but the pustules are really quite fragile. This is due a glucagon secreting tumour of the pancreas. The rash is typically seen in the perineum, buttocks and groin. You get a psoriasiform hyperplasia but a classic feature is pallor of the cells of the upper epidermis and this same picture is also seen in acrodermatitis enteropathica and they may have common neutritional deficiency based etiologies. There is usually parakeratosis overlying this pallor and sometimes some subcorneal splits. If neutrophils invade the subcorneal splits it gives rise to the pustules at the advancing edge of these lesions.
View this Virtual Slide of Necrolytic Migratory Erythema
Acute Generalised Exanthematous
Pustulosis is very similar to pustular psoriasis. Again there are mainly subcorneal pustules,
although the pustules may also be intraepidermal. There is also a bit of spongiosis at the
margins and quite a bit of exocytosis and neutrophils from the dermis up into
the epidermis to the pustules. In this
condition though, there is also a fair number of eosinophils because it is a
form of allergic drug reaction. If
you see this it helps to distinguish acute generalised exanthematous pustulosis
from pustular psoriasis. Patients with
this condition are usually quite ill, with fever and often have a peripheral
leukocytosis as well. The pustules
develop on a red base and are particularly prominent in flexural areas.
View this Virtual slide of Acute Generalised Exanthematous Pustulosis
View this Virtual slide of Acute Generalised Exanthematous Pustulosis
The last pustular disorder to consider in infants is infantile acropustulosis. Now, this disorder is often seen in infants who have had scabies, because pustules of the palms and soles are quite common as a reaction to infantile scabies. Again it is an intraepidermal pustule with neutrophils, occasionally with some eosinophils and it can subsequently go up to be a subcorneal pustule. There are no bacteria or fungi seen and often it is difficult to visualise any scabies mite either. This problem can persist after infantile scabies has been cured.
In summary, with pustular
disorders look to see where the pustule is. The majority are going to be intraepidermal or
subcorneal. Look to see if it is mainly
neutrophils or if there are eosinophils as well.
If it is mainly eosinophilic in a child consider transient neonatal
pustulosis or Incontinentia pigmenti if there are lots of eosinophils and it is
more prominent on the limbs rather than on the face. In other disorders look to see if the
pustules are associated with any viral cytopathic changes as you would expect to see
with herpes virus. Look to see if there are neutrophils around the hair follicle as you would get in a staph
folliculitis. Look also to see if there
is dermal involvement as in Majocchi's granuloma where there is a neutrophilic
reaction to fungi in hair follicles and also see if there are any other
epidermal changes as with the pallor that you get in the upper layers of
the epidermis in acrodermatitis enteropathica or necrolytic migratory erythema
in the glucagonoma syndrome.
View the video below on Sub corneal Pustular Disorders